Far from a fad diet, the ketogenic diet, a.k.a the keto diet, is proving that it is here to stay. The attention is well justified, since the ketogenic diet has benefits for athletes, weight loss, and several other health-related conditions. And with an emphasis on the consumption of whole, nutritious, tasty foods, many people find the diet to be fairly non-restrictive. In fact, some claim they’ve never eaten better. They don’t even miss the carbs which were once a staple of their low-fat diet.
But, the keto diet is more than just chugging buttered coffee and blending MCT oil into your post-workout smoothie. If you’re thinking about starting a ketogenic diet anytime soon, there are many things to understand about how the diet plan works (and why it’s so effective). Let’s take a deep dive into the keto diet and how it works.
The What and Why of Ketosis
Ketosis is a physiological state defined by the presence of ketone bodies in the blood. Ketone bodies can be thought of as an energy source for the body, just like carbohydrates and fat.
Many tissues in our body can use ketones. You might be thinking, “what’s the use of ketones, if we can just use carbohydrates and fat?”
Ketones are often thought of as an “alternate” energy pathway; the human body evolved to create ketones in order to survive times of low energy availability.
For example, when carbohydrates in the form of glucose and glycogen (the stored form of glucose) are depleted, a cascade of signals is initiated in the liver that ultimately results in the production of ketone bodies from fatty acids. There are three main ketone bodies: acetoacetate (AcAc), beta-hydroxy-butyrate (BHB), and acetone.
In times of real starvation or starvation-mimicking conditions (like prolonged fasting or very low carbohydrate diets), ketones become a fuel source for the brain and skeletal muscle since blood sugar is low. This may allow sustained performance and function. Thanks to our prodigious amount of stored fat, our ability to tap into this source of energy is nearly limitless. The ability to enter into ketosis is in everyone, we just have to allow the body to achieve it. One important side note. Be careful not to confuse physiological ketosis with ketoacidosis, which is actually a pathological condition sometimes encountered in people with diabetes.
Ketosis is where the “keto” in “ketogenic diet” comes from.
Ketogenic diets are designed to produce a state of ketosis—this comes from consuming high amounts of fats (from which ketones can be produced) along with restricting carbohydrates to <50g/day.
The ketone bodies AcAc and BHB, which are produced in response to a ketogenic diet, are shown to have beneficial signaling properties throughout the body; these benefits include enhanced longevity, improved healthspan, and treatment of neurological disorders and obesity.
However, as we will see, you don’t have to be “ketogenic” (producing your own ketones) to be in ketosis.
Ketosis can also be achieved through outside means; this is termed exogenous ketosis. Both exogenous ketosis and endogenous ketosis (meaning, the body produces its own ketones through diet or fasting) can unlock some of the benefits we just mentioned. Let’s take a look at how to get there.

How to Achieve Ketosis
First off, let’s define ketosis.
A generally accepted “threshold” for ketosis is a blood level of BHB above 0.5 millimolar (mM).
Traditionally, physiological ketosis is achieved through fasting or carbohydrate deprivation. After a long enough time, blood glucose starts to drop, glycogen stores become depleted, and the body begins to find other routes of energy production.
Exogenous Ketone Supplements
As an alternative to achieving ketosis through fasting or a ketogenic diet, exogenous ketone supplements can be used to induce ketosis.
Exogenous ketones can come in forms such as ketone salts and more commonly, ketone esters such as the BHB monoester. Ingesting exogenous ketone esters has been shown to induce physiological ketosis without a ketogenic diet or fasting, with levels reaching up to 6mM.
Alternatively, ketone salts might boost ketone levels to around 0.6mM.
While supplements induce more short-term ketosis and thus may provide improved mental clarity and athletic performance, exogenous ketone supplements may not grant the same health benefits achieved through diet and/or fasting, since your body won’t be burning its own fat.
Fasting
Intermittent fasting (IF) is a popular practice, with iterations of IF including narrowing the eating window of the day, alternate day fasts, water-only fasts, and prolonged 3 - 5 day fasts.
While many people fast for reasons such as a “gut reset” or to strengthen will power, one of the main benefits of fasting is that it is a potent inducer of ketosis, and it’s also great for weight loss.
After an overnight fast you might not be in full-on ketosis, as ketone levels might show 0.1mM - 0.2mM. However, longer fasting periods lead to higher ketone levels, up until a maximum of about 8mM - 10mM.
One study found that after two days of fasting, BHB levels in a healthy adult brain was 0.6mM; following three-day fast, levels rose to 0.98mM. In this study, brain BHB correlated well with plasma BHB.
The ability to enter ketosis through fasting, however, will also depend on other factors like how much you exercise and how long your fast is. Furthermore, when paired with dietary strategies, ketosis might be achieved sooner with higher ketone levels.
Ketogenic Diet
The final way to induce ketosis is through dietary carbohydrate restriction, a.k.a a very low-carbohydrate ketogenic diet (VLCKD) also known as a ketogenic diet (KD). While similar to the Atkins diet, keto is a bit different. The Atkins eating plan advocates high protein consumption, while keto recommends a more moderate protein intake. Other misconceptions about keto are that it's "just another low-carb diet" or that keto is paleo. Neither of these statements is correct.
Ketogenic diets involve dietary carbohydrate restriction paired with an increased consumption of dietary fat, with the remaining dietary energy coming from a moderate intake of protein. The high-fat consumption provides substrate for ketone body production by the liver, and the elimination of high-carb foods helps eliminate readily available glucose in the body, which provides the signals necessary to put the body in a ketogenic state.
In contrast to exogenous ketone supplements or fasting, a ketogenic diet might be an ideal long-term lifestyle strategy. Many find that implementing this diet is relatively simple after some time, and even find it enjoyable—doesn’t sound like a “diet” in the traditional sense of the word, does it?

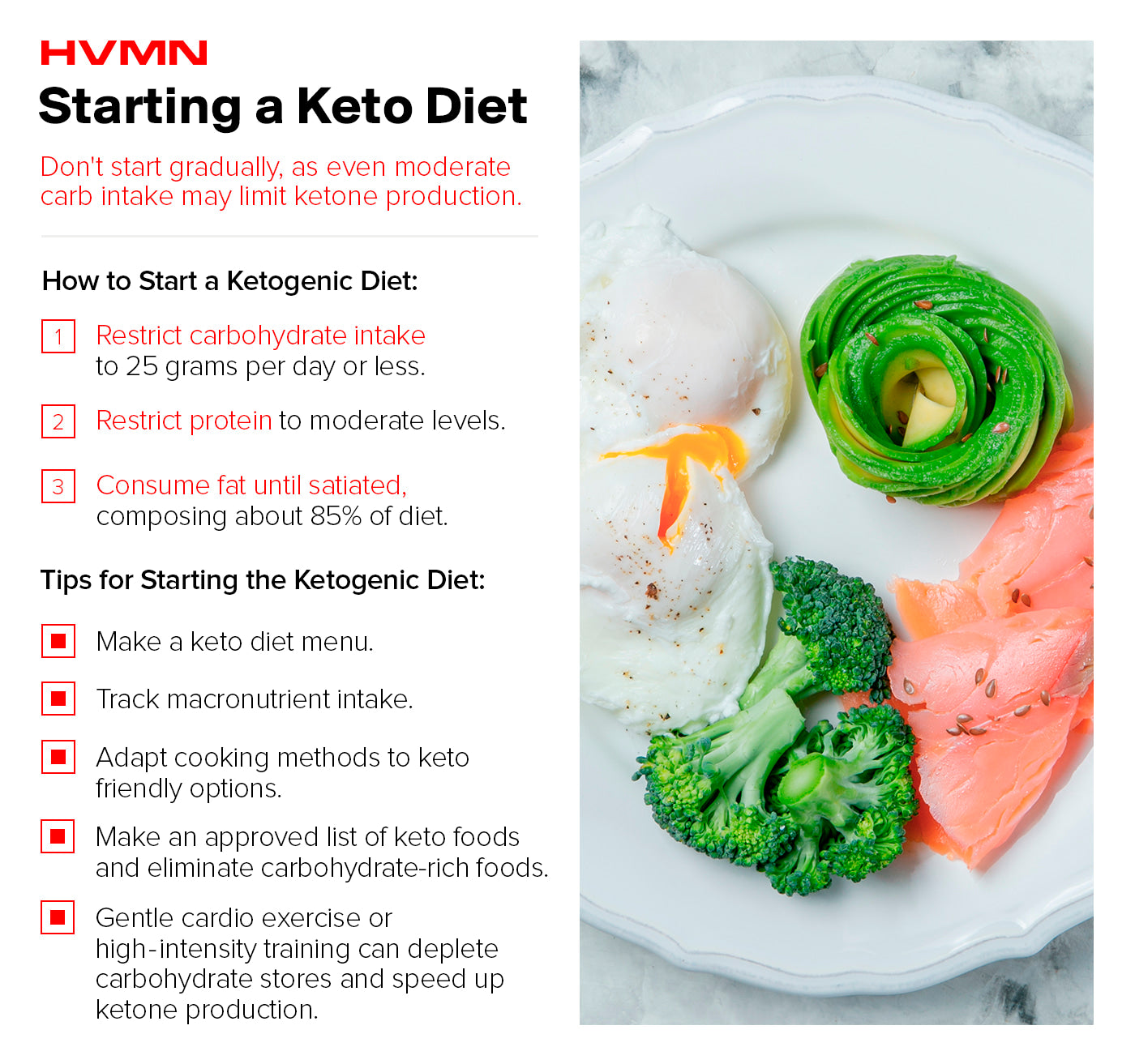
Starting a Ketogenic Diet
Since the main objective of keto is to cut out carbohydrates, the first tip would be to find and eliminate the major sources of dietary carbohydrates in your diet. You should keep total carb intake to around 50g per day or less.
The removal of a larger macronutrient in your daily diet (in this case, carbohydrates) will require that it’s substituted for something else in order to maintain caloric intake. That’s where fat comes in.
A recommendation for all keto-dieters is to eat fat until satiated (which might not take long, as fat is inherently satiating). Along with increasing your fat intake, try to integrate a good amount of fiber into your diet, particularly from leafy green and cruciferous veggies (like broccoli and cauliflower) as they are also low in carbohydrates. More starchy vegetables like potatoes are generally excluded.
As for protein, aim for about 0.5g of protein per lb of body weight (or 1g per kg, if you prefer the metric system). Athletes and individuals trying to lose weight might want to up this number a bit more.
Don’t worry about calories just yet. However, if you’re not seeing results on keto after several weeks or months, it could be beneficial to asses the number of calories you’re consuming and adjust from there.
A second tip: make a keto meal plan and a shopping list.
For those new to keto, going to the grocery store might be an intimidating experience. You’ll be purchasing many products you never have before, and not buying many things that were once staples in your shopping cart.
Having a prepared list will help you buy only the foods you need , and only those that fit within your keto diet framework.
After you shop, heaving a meal-prep strategy is also a good tip. Preparing weekly meals beforehand and packing food and snacks to take with you to work or the gym is vital. This will eliminate the temptation to buy a non-keto snack from the vending machine or have pizza delivered when you’re feeling hungry.
Initially, track your macros using an app such as MyFitnessPal or an online keto diet calculator. Tracking will allow you to see what and how much of each macro you’re consuming to make sure that fat intake is adequate and carbohydrate intake is adequately...inadequate. For many people, having something to quantify is pleasing, and helps with dietary compliance and maintenance.
Do a search for keto recipes online, become familiar with the popular keto-approved foods and ingredients, and experiment with different kinds of cooking methods. High fat consumption on keto might require that you change up dietary staples and food prep methods.
For instance, upping the use of oils like olive oil and coconut oil is a must. Adding heavy cream, butter, and cheese to dishes—something you might have once avoided—might become a daily occurrence. Fortunately, many high-fat options can be seamlessly (and deliciously) integrated into meals you’re already eating.
The Transition Period
Before going full-bore into a low-carb high-fat diet, you might want to experiment with a few things early on which can “prime” the body for ketosis and make the transition a bit easier.
The first might be simply reducing your usual carbohydrate intake for a few weeks before starting keto. Rather than go straight to 50g or less, wean off carbohydrates, maybe eating 100g one week and 75g the next, until you reach 50g and begin a strict ketogenic diet. This will make the sharp cut in carbs less drastic. Some people even keto diet cyclically, and you can also take this approach in the onset of your keto adventure.
Consider starting out with a smaller 16 - 36 hour fast or some endurance exercise first thing in the morning. All of these will deplete muscle glycogen stores quicker and help your body become more adapted to utilizing the pathways involved with using fat for energy, which can jump start ketosis. Another way to begin a ketogenic diet already in ketosis would be to use an exogenous ketone supplement.
“Getting back into ketosis with ketone esters makes a big difference. It helps get me back on track and powers me through my day.” — Lidice F.
Especially if you’re in-and-out of the ketogenic diet, ramping back into nutritional ketosis can be difficult (and could spell you with a brief bout of the keto flu). Exogenous ketone esters enables your body to run on ketones while it works toward producing its own ketones from fat stores.
“Can I Cheat on My Ketogenic Diet?”
The short answer is no. Rather, you can, but you’ll get caught.
Consuming foods that are high in carbs can and will quickly stop ketone production by the liver.
Depending on how many times you’ve been in ketosis before, it might take a considerable amount of time to get back into ketosis. This will depend on other factors like exercise, carbohydrates consumed, and how adapted your body is at producing and utilizing ketones. Stay loyal.
Measuring Ketones on a Ketogenic Diet
Your diet is on point...or so you think. If you want a way to verify that you’re actually in ketosis, several ways exist to measure ketones and the different “levels” of ketosis.
It might be good to have some objective feedback every once in a while. Three primary measuring techniques exist, each with their own advantages and disadvantages
The first method involves blood testing. This is the most accurate method for ketone testing and measures BHB—the ketone that is most abundant in the blood. However, blood testing requires purchasing a blood BHB meter along with test strips, which can get expensive. And if you’re against pricking your finger to get a droplet of blood, this testing method might not be for you.
A second method involves urine testing for ketones. Urine testing is designed to measure acetoacetate (AcAc) excreted in the urine. Since it doesn’t measure BHB, however, it may not be the most accurate or robust way to measure ketones.
The urine test strips are simple; place the stick through a stream or sample of urine, wait a few seconds, and then match the color on the strip to the color swatch on the bottle, which will give an objective measure of ketosis (that’s a range rather than an exact number). It is important to note that the ketone level measured here is a measure of what your body is excreting, and doesn’t give a picture of ketone use.
Furthermore, urine testing can be influenced by hydration status and even your level of “keto-adaptation.”
A final technique for measuring ketones involves using a breath ketone meter. These are relatively new consumer products designed to measure the level of acetone excreted in the breath, thus giving results that supposedly correlate with your level of ketosis. To date, there are very few studies that have validated breath ketone meters for accuracy.
Nonetheless, this non-invasive and highly convenient technique might be the perfect ketone-measuring tool for those new to a ketogenic diet.

Macronutrient Composition on a Keto Diet
Macronutrients (“macros” for short) are the components of food that we consume in large quantities that provide energy in the form of calories—fat, protein, and carbohydrates.
Macros provide the bulk of our body’s energy, and all of the food we consume contains some relative percent of each. We often express dietary macros in terms of what percentage of total caloric consumption they provide. For example, for someone eating a 2,000 calorie/day diet containing 80g of protein (320 calories), this would mean that 16% of their daily intake is coming from protein.
The “classic” or “standard” ketogenic diet contains around 70% - 80+% of total calories from fat, 10% - 15% from protein (more liberal keto diets sometimes will have 20% - 25% kcals from protein), and 5% - 10% or less from carbohydrates. Alternatively, the classic ketogenic diet can also be thought of as containing a 4:1 ratio of fat to protein and carbohydrates, respectively.
In this instance, if you took a moderate caloric intake of 2000 kcal/day, a macronutrient composition consistent with classic keto would contain around 155g of fat, 100g of protein, and less than 50g of carbohydrates.

Carbohydrates
The word “carbs” now comes with a stigma attached to it, but contrary to popular belief, carbohydrates aren’t “toxic” per se. In fact, carbohydrates serve as one of the body’s preferred sources of energy, particularly for high-intensity activity.
Glucose (what carbs eventually get broken down into) has many functions in the body—it’s an energy source for the brain and red blood cells and helps replenish muscle glycogen in the muscle and liver after exercise.
We also have to maintain a certain amount of blood glucose just to stay alive and functioning. But this doesn’t mean that dietary glucose is necessary.
As it turns out, our body can manufacture glucose from non-carbohydrate sources (protein and fat) through a process known as gluconeogenesis (GNG). Even in the presence of low glucose and glycogen (like during a ketogenic diet) our body finds a way to produce the glucose necessary for vital functions.
The Dietary Guidelines for Americans recommends that individuals consume 130g carbohydrates per day, which equates to about 45-60% of calories coming from carbs. This is drastically different from a ketogenic diet, in which 5% - 10% or less of total calories come from carbohydrates. So why do carbs inhibit ketone production? Because insulin levels in the body halt the liver from producing ketones. What raises insulin levels? Dietary carbohydrate.
Carbs on keto have a few considerations, like net carbs and the glycemic index (GI) of the carbs you eat.
“Net carbs” is the total amount of carbs contained in a food minus the grams of fiber. This is proposed to be a better metric of how many carbohydrates are actually absorbed by the body for any particular food.
Because dietary fiber is not entirely broken down in the small intestine, it may not raise blood glucose levels in response to a meal.
The glycemic index (GI) of a food is a scale designed to indicate how quickly and to what extent a particular food raises blood glucose after it’s consumed. The scale goes from 1 - 100; for reference, white bread is pure glucose and has a GI of 100. Similar to foods that are high in fiber, low-GI foods might have little effect on blood glucose.
These concepts both indicate why some cruciferous vegetables and leafy greens are OK when it comes to the ketogenic diet. With a generally low carbohydrate composition, low GI, and high fiber content, they’re nutritious additions to a well-formulated KD.

Protein
Often associated with muscle-building, proteins are large molecules composed of amino acid (AA) chains.
Protein is vital for life, required for building structural and functional components of cells. In contrast to carbohydrates and fat, protein in its natural form is rarely used as an energy substrate by the body. Unless it’s absolutely necessary, our body prefers not to touch proteins for energy.
While fat is prioritized on keto, protein still plays a supporting role.
For one, amino acids can be used in a crucial process known as gluconeogenesis, where they are used to produce glucose. Why is this necessary? Well, when no carbs are consumed, the body still needs some way to give the small amount of glucose needed to provide energy for organs that can’t use ketones or fat as a fuel. On a low carb diet, a process occurs that takes the breakdown products of protein and creates glucose from them. Having enough dietary protein to meet this need is critical.
In addition, consuming enough protein on keto helps to maintain (and perhaps increase) muscle mass—if that’s your goal. Sufficient protein intake (10% - 15%) will likely allow you to maintain muscle mass while on a ketogenic diet. This equates to a target intake of about 0.8g - 1.2g of protein/kg of body weight.
One reason for this more moderate recommendation is that for some people, too much protein can increase gluconeogenesis to such an extent that blood glucose rises enough to kick the body out of ketosis.
However, this concept is largely debated, and some studies have shown that even under “optimal” gluconeogenic conditions, dietary protein from a meal contributed little to postprandial endogenous glucose production.

Fat
Fats have several physiological functions, including aiding in the formation of cell membranes and comprising other structural and functional components of our body. Our brain is nearly 60% fat—indicating that rather than a nutrient to be feared, fat is something to be embraced.
Contrary to long-held belief, fat consumed in food DOES NOT equal the fat molecules in our body. Our body fat, known as adipose tissue, is the storage form of fat found in lipid droplets inside fat cells known as adipocytes.
Fatty acids (FAs) are molecules composed of chains of carbon atoms of varying lengths. Triglycerides are fats that come from the food we eat, and are composed of three fatty acids and a glycerol molecule (“tri” meaning “three” and “glyceride” indicating a glycerol backbone to which the fatty acids are bonded).
On a ketogenic diet, fat becomes the main substrate for energy production. This is because ketone bodies are produced in the liver following the breakdown and release of fat molecules and fatty acids into the circulation.
Once carbohydrates are restricted, low insulin serves as a trigger for the breakdown of fatty acids from our internal stores (lipolysis). Once released into the circulation, fatty acids can travel into the liver, where they are then used to produce ketones (ketogenesis) by the liver mitochondria.
This process requires sufficient fat be provided via the diet to provide substrates for ketone production. Aiming to get a majority of your calorie intake from high-quality sources of animal and plant fat becomes a focus of the keto diet.

Micronutrients on Keto
While macros are the focus on keto, this doesn’t mean micronutrients should be kicked to the curb.
In fact, micronutrients may be a crucial consideration on keto, given that, at least initially, this diet can throw off the body’s balance of several key minerals which help with vital physiological processes and are necessary for optimal health and wellness.
Why worry about micronutrients? Well, cutting out carbs on a ketogenic diet can lead to the elimination of many foods that are rich in micronutrients—primarily fruits, veggies, and fortified grains.
This isn’t to say that keto foods are LOW in micronutrients, just that many foods rich in micronutrients are also high in carbohydrates, and thus eliminated on a ketogenic diet.
Additionally, carbohydrate restriction has a diuretic effect, increasing urine production and a “shedding” of body water. But water isn’t the only thing lost in this process—minerals and other micronutrients are excreted as well.
The primary micronutrients to be aware of are sodium, potassium, magnesium, and calcium.
These are known as electrolytes, and they play roles in things like maintaining blood volume, cell membrane potentials, muscle contraction, and proper function of the heart. Deficiencies in these minerals are associated with numerous health issues.
Sodium
Sodium, often synonymous with salt (which is actually sodium chloride; NaCl) is an essential nutrient that helps with blood volume and blood pressure maintenance, maintaining electrical membrane potentials in muscle and heart cells...and making food taste great.
Sodium loss may occur on a ketogenic diet since under conditions of low insulin, the kidneys absorb less sodium and excrete more into the urine.
For this reason, adding more salt to your ketogenic diet might be a good idea, especially if you’re feeling symptoms like dizziness, fatigue, or muscle cramps or spasms. While sodium recommendations specific do keto don’t exist, studies on ketogenic diets in athletes have supplemented the low-carb diets with 2 - 3g of sodium per day — often in the form of bullion.
Adding salt to your diet in the form of bone broth, bouillon, or just shaking some onto meats and vegetables is a great way to up your intake.
For individuals with high blood pressure who may also be salt-sensitive, consult a doctor before increasing sodium intake.
Potassium
Potassium is necessary for proper muscle contraction and blood pressure regulation, among other functions.
The recommended intake for potassium on a ketogenic diet is around 3g - 5g per day. Prioritizing keto-friendly potassium-rich foods is a must. Some of these include: beans and peas, avocados, green and root vegetables, and nuts.
Magnesium and Calcium
These two minerals might not necessarily fall drastically on a ketogenic diet, but are nonetheless important to maintain health and function.
In particular, magnesium deficiencies are now being proposed as one reason for the increased prevalence of cardiovascular disease in the U.S and around the world.
Calcium is known to promote “strong bones and teeth” but is much more complex than just that.
Calcium is needed for blood clotting, cell signal transmission, and blood pressure regulation.
Being aware of what happens to micronutrient levels on a ketogenic diet can allow you to take precautions. Prioritizing micronutrient-rich, keto-friendly foods and perhaps using a mineral supplement are two ways to prevent micronutrient deficiencies.
Obviously, attaining your nutrients through whole-food sources is ideal, because nutrients in food are often more bioavailable than isolated nutrients from supplements or pills. Food nutrients are consumed in conjunction with other beneficial polyphenols, antioxidants, and carotenoids that probably all require one another for optimal efficacy. But sometimes diet isn’t enough, and supplementation can become beneficial.

The Best Keto-Friendly Foods
While we aren’t here to provide a comprehensive keto recipe book, it might be good to get an idea of what kinds of food you can consume on a ketogenic diet (in some ways, this will also tell you what you CAN’T consume).
In the produce section, several options exist. Look to consume a variety of colorful vegetables; including but not limited to dark leafy greens like kale and chard, mushrooms, broccoli, cabbage, brussels sprouts, peppers, asparagus, zucchini, eggplant, and other herbs. Throw these in a pan with some coconut oil and you have a high-fat veggie feast.
Oh, and while technically a fruit, avocados are a high-fat, tasty option that can keto-fy just about anything (just skip the toast).
Some high-protein, no-carb options in the meat section include grass-fed meats like beef, lamb, pork and veal, fatty fish, oysters, scallops, crab and lobster (for the seafood fans out there), pasture-raised poultry, cage-free eggs, bone broth, and organ meats.
Other great sources of protein and fat include full fat dairy like cheese and whole milk. A favorite of many keto-dieters is ghee, a form of clarified butter that goes well in coffee.
When looking for healthful sources of fat, oils make the cut.
Olive oil, coconut oil and avocado oil are all great oils to cook with. In addition, grass-fed butter, nuts, and seeds can become staples in a ketogenic diet.
You may find it difficult to get high-quality fats on a keto diet through whole-food sources alone. Supplements can help you out here. MCT oil and MCT oil powders might be something to look for. You can use them to boost coffee, shakes, and even smoothies and other keto snacks.
Are Sweeteners OK on Keto?
As long as they are low-to-zero-calorie, the answer is yes.
Several sweeteners including stevia, erythritrol, and monk fruit comprise some keto-friendly sweetener options. By “keto-friendly,” we mean that these “non-nutritive sweeteners” (NNS) don’t lead to spikes in blood glucose or insulin after they’re consumed, so they won’t halt ketone production.
So, if you want to sweeten up your morning coffee or make some keto baked goods, calorie-free sweeteners have the green light from a keto perspective.
Keto Diet Considerations
Many swear by keto, but just like other diets, it isn’t for everyone. The important things to consider when deciding whether or not to “go keto” are your current health status, your health goals, and how (and if) keto can fit into your life.
Who should avoid keto? There are certain metabolic conditions where the ketogenic diet is advised against. These include pregnancy, kidney failure, impaired liver function, impaired fat digestion disorders (gallbladder disease, gastric bypass, pancreatitis), and genetic defects in metabolism such as CPT I/II deficiency, beta-oxidation defects, or fatty acyl dehydrogenase deficiency.
If you happen to have a medical condition which could be positively or negatively affected by keto, it’s best to first talk to your doctor before making any significant dietary changes.
Potential Side Effects
For most people, carbohydrates have been the preferred and only source of oxidizable energy for most of their life. This means that we may lack the necessary machinery to properly produce and take advantage of ketones. Because of this, starting a ketogenic diet may come with some side-effects, colloquially referred to as the “keto flu.”
It’s not a viral infection. The keto flu is a series of symptoms that can occur in the initial 2 - 3 days after starting a ketogenic diet.
Blood glucose will be low (due to lack of carbohydrate consumption) but ketone production won’t quite yet be optimal enough to provide fuel for the brain, leaving it “starved” of energy. The initial stages of keto can also lead to rapid loss of body water, which takes essential minerals with it. This electrolyte imbalance can lead to some unpleasant symptoms such as nausea and dizziness. Due to the body sensing a “starvation response,” hormonal changes can also occur, such as an increase in cortisol.
Symptoms of the keto flu include headaches, muscle cramps, fatigue, nausea, dizziness, low mood, fatigue, and cravings.
Symptoms of the keto flu will vary in severity and intensity on an individual basis, and some may not experience symptoms at all.
As keto adaptation takes place and your metabolism shifts, you’ll be able to produce ketones and use ketones and fat more readily as a fuel source—this might take anywhere from a few days to a few weeks to fully occur.
However, as your potential to use fat increases, symptoms should subside, and you’ll begin to feel the benefits of ketosis for yourself. These benefits might include increased glycogen conservation during exercise, increased ability of muscles to use fat and spare ketones for the brain,
But these physiological effects aren’t the only benefits provided by a ketogenic diet.

Non-Medical Applications for Ketogenic Diets
The utility of ketosis doesn’t end at the original application for epilepsy. Whether the goal is to improve body composition or run a bit further, ketogenic diets might have some application.
Appetite Control
Perhaps one of the most well-observed “side effects” of a ketogenic diet is the reduction in appetite and anecdotal claims of increased satiety.
This may be due to the emphasis on fat and protein consumption—two macronutrients that are thought to be highly satiating (they make you feel full). Indeed, ketogenic diets have been shown to increase satiety and decrease feelings of hunger.
This effect might be due to more than just macros. Ketones may have appetite-suppressing properties themselves. The ketone body BHB, when taken as a ketone ester, suppresses ghrelin, the hunger hormone, and reduces perceived hunger and the desire to eat.
A ketogenic diet may allow you to control your hunger, rather than have your hunger control you. In this way, this dietary approach seems to empower many individuals who are no longer subservient to their food cravings.
Athletic Performance
There seems to be an ongoing debate on which diet is best for performance.
Carbohydrates have long been prioritized as the fuel for high-intensity performance, and not much has changed in this realm.
However, there is an increasing interest in the use of ketogenic diets in the world of athletics, particularly those involving body composition concerns or requiring extreme endurance.
Since ketogenic diets increase the ability for athletes to burn fat,
While some studies have shown enhanced endurance capacity following a ketogenic diet,
Results will be context dependent and highly variable among athletes.
While moderate-intensity endurance sports and some strength and body-composition dependent sports may show increases in performance on keto, higher-intensity efforts may not receive the same boost.
Future research on ketogenic diets, particularly in athletes practicing them long term, may provide more answers and efficacy for this regimen.
Clinical Applications for Ketogenic Diets
The first medical use for ketogenic diets was treating epileptic seizures. Since its initial application in 1921, keto has come a long way, and is now used to treat a variety of medical conditions such as obesity and diabetes and treat risk factors for things like heart disease.
Weight Loss
Ketogenic diets have been shown to be superior for weight and fat loss and weight loss maintenance when compared to traditional low-fat, high(er) carbohydrate diets.
A big contributor might be the aforementioned appetite-suppressing effects of the ketogenic diet. Reduced hunger can lead to fewer calories consumed, which will lead to weight loss in the long term and help keep weight off. But calories aren’t the only thing that matters.
Ketogenic diets may also benefit weight loss due to their proposed “metabolic advantage.”
This is perhaps due to the thermogenic effect of protein (it takes more energy to digest protein than other macronutrients) and an increased energy expenditure due to the ATP requirements of gluconeogenesis. Hormonal changes may also play a role, as ketogenic diets lead to reduced signaling for fat storage that comes with low insulin levels.
Type 2 Diabetes
The metabolic abnormalities of impaired glucose tolerance and reduced or impaired insulin sensitivity may be improved by ketogenic diets.
A high-fat diet is being increasingly recognized as a first-line treatment for diabetes.
Perhaps one of the largest studies to date was led by VIRTA health. It was a 2-year trial that illustrated nutritional ketosis achieved through a ketogenic diet can improve multiple biomarkers of diabetes and cardiometabolic risk. The diabetic patients also lowered their medication use, and several in the study population completely reversed their diabetes and visceral obesity.
Cancer
In some cancers, growth is potentiated by glucose availability, which provides energy for the tumor.
Although not universal, aerobic glycolysis (breakdown of glucose using oxygen) is a feature of many cancers, and insulin may facilitate the uptake of glucose into cancer cells. For this reason, it has been proposed that ketogenic diets may have anti-tumor effects due to their ability to lower glucose and insulin.
One study with 10 human subjects, scientists showed that an insulin-inhibiting diet (i.e. a ketogenic diet) was safe and feasible in a set of patients with advanced cancer, in whom the disease was kept stable or even went into partial remission.
In a case study involving two pediatric oncology patients, seven days of a ketogenic diet decreased blood glucose levels, and scans indicated that there was a ~22% reduction in glucose uptake by the tumors in both subjects.
Of course, cancer is complex and no one solution exists for its treatment or prevention.
Neurological Disorders
Altered brain metabolism is a feature of several neurological disorders including Alzheimer’s disease, Parkinson’s disease, and Epilepsy.
The benefits of a ketogenic diet for these conditions is thought to result from the fact that ketones provide an alternative fuel source to glucose, and could alter pH levels in the brain, which directly affect ion transporters and neuronal receptors.
The results speak for themselves.
Ketogenic diets have shown success in reducing the frequency of seizures in children with epilepsy,
There are even some case studies indicating that ketogenic diets might be beneficial for sufferers of migraines.
It is important to recognize that ketogenic diets are not yet recognized as first-line treatments for any of the above disorders.
Yes, a ketogenic diet is a relatively easy intervention to implement, is tolerable, and may be much more enjoyable than medication or surgery, but everything is in stage one right now.
As data becomes more robust, perhaps doctors and patients alike will begin to notice the potential of ketogenic diets to enhance health and reduce disease burden. More studies are needed in a larger amount of patients to determine the real efficacy of ketogenic diets for disease.
Is Keto for You?
The case for keto is strong.
If you’re looking for a dietary change that will still allow you to consume foods you enjoy while experiencing improvements in health, the ketogenic diet might be for you. Research on this diet seems to be increasing at the same rate as the web searches, so it’s likely more data on keto will keep getting published in the near and far future, perhaps providing even more robust evidence as to the diet’s efficacy. Sure, there are criticisms. Many claim that too much saturated fat on keto could raise LDL cholesterol levels and other disease risk factors. Most research, however, has yet to show long-term harms from clinical use of the ketogenic diet.
With the knowledge of the benefits and risks, the “dos” and “don'ts”, and empowered with scientific research, you can begin to formulate a ketogenic diet that fits into your lifestyle.
Editors Choice

How to Get Into Ketosis Fast
The low-carb, high-fat keto diet has been shown to improve body composition and increase endurance performance. But getting into ketosis is difficu...

Ketones in Urine: All You Need to Know
Monitoring ketone levels in urine is important for both diabetics and those waiting to maintain ketosis. Here's what to look for, how to test and t...

VO2 Max: Training to Use Oxygen Efficiently
VO2 max might be the truest representation of endurance fitness there is. While elite runners and cyclists train their bodies to use a high volume ...

Do Calories Matter on a Keto Diet?
Are all calories created equal? Not on the keto diet. Weight loss has emerged as a primary incentive for going keto. That's not driven by the amoun...

Keto Diet Fundamentals
A ketogenic diet, or “keto diet,” refers to an extremely low-carbohydrate, high-fat pattern of eating. This article dives into the history of the k...

Beta-hydroxybutyrate or BHB –All You Need to Know
BHB stands for beta-hydroxybutyrate, one of the three main ketone bodies. It's a clean-burning energy source for both the body and the brain. What'...

Ketone Salts: Ketosis with a Cost
Ketone salts, also known as BHB salts, provide the body with a way to enter ketosis. But the results are mixed. There are a few options for someone...

How to Run Faster: Mental and Physical Techniques
Runners chase speed. For many, it's a lifelong pursuit. The connection between the body and the mind is important for speed, and harnessing both wi...



